
Most women have breast discomfort at some stage. Often pain develops in the days just before a period. Pain is generally mild, but it can be severe, affecting quality of life, physical activity, lying on your side/front. Hugging and sexual activity can be uncomfortable.
Evening Primrose/Starflower Oil could be worth trying.
Before starting HRT a full health assessment is necessary to assess any health conditions which may need to be taken into account when considering which type, regime and route of HRT to recommend. It’s also important to understand which symptoms are causing most concern and what each woman’s expectations of HRT are. Lifestyle, working patterns and individual preferences also need to be considered.
Over time, many women become aware of a ballooning or bulging of the vagina walls, or the uterus (womb) sitting lower in the vagina. Others describe a heavy dragging sensation low in the pelvis. These are all signs of prolapse.
The pelvic floor muscles are a broad sling of muscles, like a trampoline, stretching from the pubic bone at the front of the pelvis to the coccyx (tail bone) at the back. They form the floor of the pelvis and are responsible for:
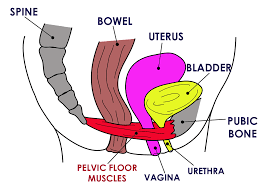
- Supporting the pelvic organs - bowel, bladder and uterus (womb)
- Controlling the bowel, bladder, and sexual functions
Weakness of these muscles can happen following childbirth. Also, gravity, obesity, chronic constipation and persistent coughing all put a huge strain on the pelvic floor. When the pelvic floor weakens and sags the pelvic organs become less supported and drop (prolapse). Menopause also affects the pelvic floor.
 Many women find their hair loses volume and length around menopause; hair can also become brittle, fragile and break more easily. Some women also notice hair thinning and shedding - particularly around the hairline and crown – known as female pattern hair loss (FPHL).
Many women find their hair loses volume and length around menopause; hair can also become brittle, fragile and break more easily. Some women also notice hair thinning and shedding - particularly around the hairline and crown – known as female pattern hair loss (FPHL).
Common signs of menopausal hair thinning:
Ponytail is thinner
Hair not growing as long as it used to
Parting is wider and scalp is more visible around the crown
Recession and/or thinning at temples
Reduced thickness and length of each strand
These changes can be really stressful since our hair is a very important aspect of our identity. Other unwelcome changes to our appearance may also be happening around the same time, leading to further distress…
 Bioidentical HRT appears to be readily available and easily accessible, but is it safe, and what’s the difference?
Bioidentical HRT appears to be readily available and easily accessible, but is it safe, and what’s the difference?
Most bioidentical hormones are derived from plant sources, as are most types of traditional, Bodyidentical, HRT - and both undergo synthetic processing in laboratories to obtain the hormones used. However, this is where their similarity ends.
First, some science - There are actually 4 main types of oestrogen in the female body: The most potent oestrogen produced from the ovaries in the years before the menopause is estradiol (E2). Estrone (E1) is the predominant, but much weaker oestrogen produced after the menopause. The fluctuating and declining levels of E2, which occur during perimenopause as the ovaries stop functioning normally, is understood to be the cause of menopause symptoms - and deteriorating heart and bone health.
Unfortunately, E1, produced post menopause, is too weak to prevent symptoms or to protect heart and bones. During pregnancy, the main oestrogen is produced from the placenta and is called estriol (E3), whilst estetrol (E4) is another oestrogen created by the developing foetus during pregnancy. Exciting research is underway to utilise E4 in HRT and contraception as a safer alternative to E2.
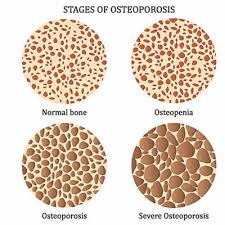
Bone is a living tissue that constantly regenerates. Complex processes throughout the body cause new bone to be laid down as old, weak bone is removed - this maintains strong bones. Until around age 30, we normally build more healthy bone than we lose, but after our 30’s, bone tissue naturally starts to decrease. With age and reduced Oestrogen levels, particularly when the menopause occurs before the age of 45, there is an increased risk of progressive loss of bone strength leading to bone thinning and fragility (Osteoporosis). Although bone loss occurs in both women and men, the loss is more rapid and is more common in women.
Approximately 10% of a women’s bone mass is lost in the first 5 years of menopause.
Hot flushes and night sweats are experienced by many menopausal women for an average of seven to thirteen years, and for some, these can last a lifetime. Women who are seeking to improve these menopause symptoms without using HRT can consider prescribable alternatives. These medicines have been developed for other medical conditions, such as epilepsy, pain or high blood pressure, but have also been found to have a beneficia l effect on some of the most common and debilitating menopause symptoms.
l effect on some of the most common and debilitating menopause symptoms.
 Many women feel that their weight gets harder to manage the older they get. We often approach menopause already struggling with our weight, and then IT JUST GETS EVEN HARDER.
Many women feel that their weight gets harder to manage the older they get. We often approach menopause already struggling with our weight, and then IT JUST GETS EVEN HARDER.
Fluctuating and falling hormone levels around menopause can affect the way we store fat. This is because our bodies want to store fat for later - a bit like "puppy fat" at puberty. We develop "insulin resistance" making our bodies store, rather than burn, calories. How the body handles food also changes: For example , if you eat 1000 calories before menopause you will burn 700 and maybe store 300. After menopause you will store 700 and burn only 300!
 Migraine tends to worsen in the years leading up to the menopause, with attacks occurring more frequently and also lasting longer. Many women notice a link with their periods. For some women, the natural drop in oestrogen that occurs around menstruation - and during the pill-free week of combined oral contraceptive pills - can be a trigger. Others find that heavy, painful periods are linked to migraine. From early 40s, the menstrual cycle can become more erratic, with fluctuations in oestrogen levels, leading to more frequent migraines. As periods lessen and become infrequent, the hormonal trigger for migraine lessens; which is why many women find migraine improves after the menopause.
Migraine tends to worsen in the years leading up to the menopause, with attacks occurring more frequently and also lasting longer. Many women notice a link with their periods. For some women, the natural drop in oestrogen that occurs around menstruation - and during the pill-free week of combined oral contraceptive pills - can be a trigger. Others find that heavy, painful periods are linked to migraine. From early 40s, the menstrual cycle can become more erratic, with fluctuations in oestrogen levels, leading to more frequent migraines. As periods lessen and become infrequent, the hormonal trigger for migraine lessens; which is why many women find migraine improves after the menopause.
 Although pregnancy is less likely during perimenopause and menopause, it is still possible. Even when periods are very infrequent (or non-existent in younger women with POI), a spontaneous ovulation can occur and result in pregnancy. Therefore, women who do not wish to become pregnant should use reliable contraception – current guidance recommends using contraception for 2 years after the last natural period if periods stop before age 50, and one year after the last natural period if periods stop after age 50. Generally at age 55 contraception is no longer required as the possibility of pregnancy would be very low.
Although pregnancy is less likely during perimenopause and menopause, it is still possible. Even when periods are very infrequent (or non-existent in younger women with POI), a spontaneous ovulation can occur and result in pregnancy. Therefore, women who do not wish to become pregnant should use reliable contraception – current guidance recommends using contraception for 2 years after the last natural period if periods stop before age 50, and one year after the last natural period if periods stop after age 50. Generally at age 55 contraception is no longer required as the possibility of pregnancy would be very low.
